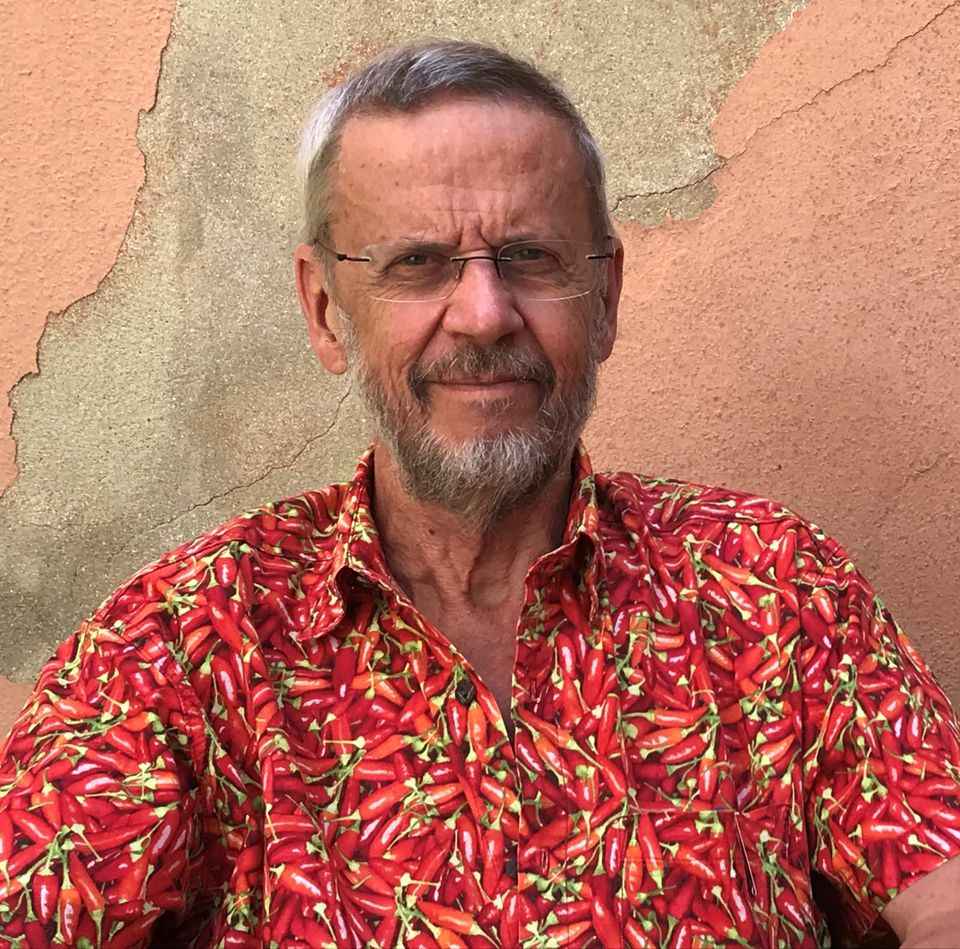
A veteran Danish anthropologist who received a doctorate in medicine for describing the effects of vaccination on reducing the rate of child deaths in the Global South have contributed to a paradigm shift twice in his life.
An academic researcher has to be always willing to be totally open-minded during any research proces. Every time the researcher finds something is hard to believe, it might be the time to return home and test once more in another setting exactly those unbelievable research results.
”The golden moment in science is when your pre-conceived ideas are contradicted by data”, says the Danish health anthropologist Peter Aaby who is famous globally for describing the effects of vaccinations on children in Guinea-Bissau.
In spite of being an anthropologist, Peter Aaby received in 1988 a doctorate in medicine from University of Copenhagen for his research. But he is definitely not a great fan of interdisciplinary academic work.”When you shift from one method to the other, your focus will weaken. I am an anthropologist, and my strong point has been my ability to be steadfast in telling medical researchers that something within their established truths has been contradicted by anthropological observations by me and others”.
”I am born in 1944, and I grew up in the shadow of the newly invented antibiotics. At that time, you were not expected to question the expertise of the universally worshiped medical science. One of the big problems within medical science – and it has only grown worse through the 44 years I have taken part – is medical researchers are only studying what is planned from the beginning. They have a hypothesis, and that is what they are testing. They don’t allow themselves to get new insights through the research proces. In that sense, anthropologists have another upbringing”.
As a young politically motivated anthropologist, Peter Aaby took part in heated political debates at his institute, and he was one of the initiators behind IWGIA (International Work Group for Indigenous Affairs), a global NGO which still has its head office in Copenhagen.
The myth of malnutrition
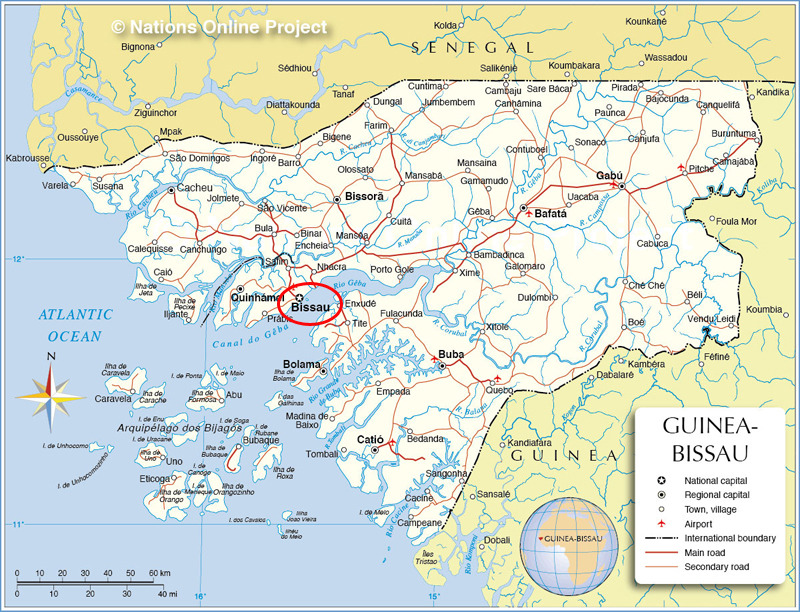
When he arrived in 1978 in recently independent Guinea-Bissau for the first time, his interest in the country was primarily political. How did the new state manage to achieve development in the ”interface between different tribal cultures and the semi-socialist thinking that had dominated the struggle for liberation?”, as he puts it.
Two years earlier, a Swedish mission had observed that the rate of child deaths in Guinea-Bissau was more than 50 percent before the age of five. According to medical science of the time, the many deaths among small children in the Global South was caused by a weak immune system due to serious malnutrition. An understanding which seemed to be confirmed by frequent hunger disasters around the globe. So the opportunity that brought Peter Aaby to Guinea-Bissau was his participation in a Swedish-funded interdisciplinary project with the purpose of mapping malnutrition among children. The participating anthropologists, including Peter Aaby, were supposed to look at food habits, especially in the countryside. Did cultural patterns influence the supposed malnutrition?
The cars that were ordered for the project’s participants were delayed. And therefore, in cooperation with the health ministry of the new state, the team began its work in the Bandim neighbourhood in the capital city instead of the countryside regions. Today, the Bandim Health Project which was later founded by among others Peter Aaby is till based in Bandim with its 160 employees, and he is still living in a modest rented apartment in Bandim most of the year.
”In November and December 1978, we examined all children in Bandim, and we found almost nobody with malnutrition. Soon after, the other team members left Guinea-Bissau, and I was the only one to continue. Already now, we could clearly see that data was contradicting our hypothesis, but in spite of that we continued surveys of the eating habits of the country’s different ethnical categories with help of local staff – all the time with an underlying sensation that something was wrong”, he remembers.
During the work, a measles epidemics happened in the Bandim area. Together with local health authorities, Peter Aaby and his team arranged public gatherings in order to educate people how to avoid being infected, but sixty children in the area died, and according to Peter Aabys observations their state of nutrition had nothing to do with who died and who did not. ”But families in which the head of household had several wives and therefore many children were the hardest hit, so we had a theory, that the reason could have something to do with the dose of virus they were receiving. We examined and gathered data about one hundred children who got infected. We could see that the death rate was higher among those infected children who had been infected in their own family”.
An absurd aha-experience
After finishing his assignment at the original Swedish-funded project in 1981, Peter Aaby got a job as assistant professor at Institute of Anthropology at University of Copenhagen. During the following years, he was teaching half of the year in Copenhagen, but asked for leave without salary the other half of the year and moved to Guinea-Bissau in order to continue his research for his own money – ”or rather no money”, as he puts it. He returned to the households in Bandim where children have had measles during the epicemic of 1979.
”We should have done that from the beginning, but it takes a lot of time to do the opposite of what you are brought up to do”, he explains. After the new survey, they had registered a total of 453 cases of measles, and these data showed two things: Nutrition had nothing to do with who got sick and who did not. And those children who died were the ”secondary cases”, i.e. those who were infected by other members of their own family with whom they were together for long time spans. This pattern was then compared with data from other epidemics in Senegal and elsewhere, and in 1983, Peter Aarø and his colleagues were finally able to publish an article about their findings in an academic journal.
Again, many doctors couldn’t imagine that the dose of virus should play such an important role. They had always learned that virus were growing so fast in an infected body that the initial dose would have less importance. Doctors representing this understanding had a lot of influence on funding for research projects around the world, so it was still difficult for Peter Aaby and his colleagues to get funding for their continued research. But at the same time their work was increasingly recognized by other donors, so the Bandim Health Project began to grow.
Gradually, the focus of research moved to the field of vaccinations. Already during the measles epidemic in 1979, the research team received a few boxes with measles vaccine from Sweden and they gave it to non-infected children of Bandim as a social measure. Later, sitting in Stockholm and trying to put together a report about the original research project, Peter Aaby had ”an absurd aha-moment” when he looked at the hollow card sheets containing their research data and realized that those children who had died from other kinds of completely different illnesses during the following years to a high degree were those who were travelling at the time of the measles vaccine effort or for some other resaon never got the vaccine.
”Those who did not get vaccinated are those who die”. Around the same time, four other studies around the world showed the same pattern.
Two paradigm shifts
According to Peter Aaby, he has ”twice contributed to a paradigm shift”. The first shift was the realization that infection intensity and dose was in fact a decisive factor for how seriously ill an infected body would be.The second shift has been the realization and description of ”non-specific effects” of a vaccine. ”My great challenge has been to convince the world that vaccines have non-specific effects”, he says.
Thus, since the mid-1980’s, most of his research has focused on describing non-specific effect of ”living vaccines” and how they are strenghtening a body’s immune defense in a broad sense. A few years after Peter Aaby’s aha-moment in Stockholm, the IMCC (International Medical Cooperation Committee) introduced in cooperation with the Bandim centre an ambitious program for vaccinating children in Guine-Bissau against infectious childhood diseases, financed by Danida through Danchurchaid.
”They wanted to do social work, that was what the money were granted for, but I wanted to use it for research. Nobody had ever researched these matters in such a scale. We simply had to use this opportunity. Together with IMCC, we created a routine. They managed to vaccinate a lot of children, and we got a lot of data”.
Today, the death rate among children has fallen dramatically in almost all countries around the world. In Guinea-Bissau, it has fallen 85 percent since the start of the Bandim centre, and a similar pattern is seen in many countries in the Global South.
”We have studied demographic data from several countries, and in the first few years following a polio vaccination campaign, we have generally seen a reduction by 20 or 25 percent of the average death rate among children. The polio vaccine has stimulated the immune system of the children. This is not about the specific illness, it is about how your are training their immune system”.
In 1989, the Institute of Anthropology in Copenhagen asked Peter Aaby to make a choice between living in Denmark or living in Guinea-Bissau. So he left his job there, moved his address to Africa, and Statens Serum Institut, a Danish sector research institute with the purpose to combat and prevent infectious diseases, became his main affiliation in Denmark instead. Statens Serum Institut took over the role of Danchurchaid in relation to the IMCC program, and Peter Aaby was named research professor at the institute in 1995, financed by the research council of Danida.
Capacity Building
Originally, the researchers at the Bandim Health Project were from Denmark and other Northern countries. ”Guinea-Bissau simply didn’t have any researchers”, explains Peter Aaby. But today most of the researchers at the center are born and educated locally.
”We got a grant from Danida’s Enreca-fund in 1994 or 1995 with the purpose of educating Guinea-Bissau’s own experts in this field. We started with eight local doctors and biologists. Not all of them managed to get masters and PhD’s, but later more people joined the program, and as a result, we have educated 13 masters and seven PhD’s. Two of them are still working at the center. They have created their own small operational unit that does operation research for international organizations”.
”The good thing is that all of them are still in Guinea-Bissau. They are consciously trained in local conditions, their expertise is local. It’s a general trend within epideomology, that you stay in the geographical area where you were educated”.
Peter Aaby is now in principle retired – with a five percent professorship at University of Southern Denmark (SDU). The Bandim Health Project is managed by two other part-time researchers from Department of Medicine at SDU, including Christine Stabell Benn, Peter Aaby’s wife and research partner through many years.
”If they were not there, the great effort at the center would not take place, and it would be harder to convince Danida and big private foundations to finance it”, explains Peter Aaby.
The Badrim Health Project is now a center with 160 people employed, entirely working with research. Most of them are constantly gathering routine data.
”We educate a large number of PhD’s, locals as well as young people from everywhere around the world. In Guinea-Bissau, we have seen a new generation who have grown up with the internet and understands and speaks much better English”.
Most of the research focus on the situation in Guinea-Bissau, but Peter Aaby has also been deeply involved in large research projects in Senegal and has worked in close cooperation with a large British research station in Gambia. ”Nowadays vaccines are still produced with the specific aim to combat a specific illness. Look at Covid-19. You are considered healthy as soon as you don’t have the virus any longer. But actually, what makes a person healthy, is a strong immune system, and I have never heard about one single university on this globe which teach young doctors how to give people strong immune systems. It should be the main task of today’s medicine, in my opinion. I havent stopped being controversial”, says Peter Aaby.
If you skew the immune system …
Through many years of research, he and his colleagues have found out that ”every living vaccine”, i.e. every vaccine that is designed as a weakened organism replicating itself and creating antibodies within your body, has a beneficial effect in your immune system, especially for women – simply because it trains and optimizes the normal functions of the immune system. Living vaccines includes measles, calmette (against tuberculosis), polio and the old form of smallpox vaccine.
”Boosting any vaccine that you have received is a good thing for training your immune system. But if a vaccine have had a beneficial effect on the immune system, it can logically have a negative effect to stop distributing that kind of vaccine. Many countries have stopped general campaigns to vaccinate against smallpox and tuberculosis because the illnesses are considered extinct or no longer a risk, and we have made efforts to describe the consequences of stopping to use these vaccines”.
Randomized studies of smallpox and calmette, partly based on the registrations at school doctors in Copenhagen from 1964 until 1976, show that children who received these two vaccinations had 46 percent better chance to survive other illnesses between the ages of 7 and 45. When you decide to discontinue vaccinating, that positive effect will naturally be lost, Peter Aaby warns.
Furthermore, he argues that his and other peple’s research tend to show that ”non-living vaccines”, where the infectious bacteriea or virus initially have been killed and is brought into the body on a small aluminium scaffolding, i.e. hepatitis, pertussis and others, might have a harmful effect in relation to other illnesses, again especially on women. ”If you skew the immune system, you don’t know what will happen”.
”Then, what kind of vaccine are the new types of MRNA-vaccine that are currently used against Covid-19 virus? Living or non-living? It hasn’t been studied yet, but I would think that they should count as non-living ….”